Radiation Therapy
TomoTherapy Radixact X9: Next-Generation Radiation Therapy in Minsk

What is TomoTherapy: the essence of the method and key differences from conventional irradiation
TomoTherapy Radixact X9 is a comprehensive radiotherapeutic system that integrates:
Thanks to the unique design of the collimator and advanced computer technologies, the Radixact X9 allows field sizes up to 40 × 135 cm, ensuring high accuracy and treatment safety.
Main Applications in the Center
The scope of application of the Radixact X9 radiotherapeutic system includes the following areas:
Total Body Irradiation (TBI)
Used as a myeloablative conditioning regimen before bone marrow transplantation in adults and children. The introduction of total body irradiation into the conditioning regimen significantly reduces the risk of disease relapse by effectively eradicating tumor cells and reducing mortality associated with donor cell rejection in cases of allogeneic and haploidentical transplants.
This technique is also used as part of non-myeloablative conditioning regimens. To reduce the radiation dose to the lungs, kidneys, thyroid gland, and eye lenses, we use the method of intensity-modulated total body irradiation.

Total Lymphatic System Irradiation
Used in non-myeloablative regimens for organ allotransplantations to reduce the risk of donor organ rejection, as well as in the treatment of severe autoimmune diseases requiring persistent, long-term immunosuppression.

Organ-Sparing Targeted Irradiation of Bone Marrow and Lymphatic System (TMI/TMLI).
In classical total body irradiation, increasing the dose is not feasible due to increased treatment toxicity. Also, total body irradiation is not applicable for elderly and comorbid patients.
To reduce the toxicity of total body irradiation as part of myeloablative or non-myeloablative conditioning regimens before bone marrow transplantation, we widely use techniques for targeted irradiation of the bone marrow and lymphatic system for patients with hemoblastoses. This technique allows for the effective destruction of malignant cells in the bone marrow and lymphoid system, minimizing the impact on vital organs and tissues by 40–70% compared to classical total body irradiation.

Radiation Therapy for Hemoblastoses
Aimed at treating patients with oncohematological diseases, including malignant lymphomas.
The figure shows the result of radiation therapy for a patient with plasmacytoma (top image - before treatment, bottom - 3 months after radiation therapy).

Stereotactic Radiotherapy and Radiosurgery
This is a special type of radiation therapy, the main difference of which is the very precise delivery of high lethal doses to the tumor in a short period of time.
This technique is often an equivalent alternative to surgical treatment or the only possible method of therapy when surgery is not possible. It is used for high-precision treatment of malignant tumors of the lungs, liver, kidneys, and adrenal glands, including metastatic foci, with minimal impact on healthy tissues.

How is preparation for radiation therapy carried out?
Modern radiation therapy is a complex multi-level process involving a highly qualified team of specialists from different fields to make the treatment as effective and safe as possible. Let's consider the stages of radiation therapy:

1. Consultation and examination
A radiation oncologist collects the patient's history, assesses their general condition, and prescribes various examinations: general blood and urine tests, biochemical blood tests, MRI, CT, PET-CT, and others. The decision to perform radiation therapy is made collectively with hematologists, surgeons, and transplantologists.

2. CT simulation
Conducted exclusively in preparation for radiation therapy. Its goal is to accurately simulate the upcoming procedure by building a three-dimensional model of the patient's body and the irradiated volume based on the obtained images, check the correctness of patient positioning, assess the effectiveness of immobilization, clarify the location of tumor tissue relative to vital organs, and ensure the correctness of equipment settings. If necessary, the radiation oncologist requests PET-CT, MRI, SPECT/CT studies to perform image fusion in the planning system for more accurate determination of the irradiation volume.

3. Radiation dose calculation
Based on the obtained data, medical physicists in the radiation therapy planning system calculate the optimal radiation therapy plan, relying on the parameters set by the radiation oncologist, necessary for eradicating tumor cells while simultaneously protecting healthy tissues. After collegial approval of the physical parameters of the irradiation plan, mandatory verification is carried out on a specialized phantom that simulates human tissues.

4. Development of a treatment plan
An individual therapy plan is created, which includes the number of sessions, frequency of procedures, and the total duration of the course.
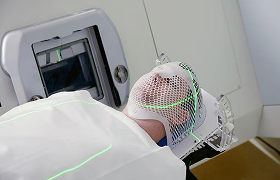
5. Selection and manufacture of immobilization devices
To ensure accurate patient positioning, both standard and individually manufactured immobilization devices are used - masks, mattresses, and fixators. They help to reliably and comfortably fix the body position, which allows maintaining immobility from session to session during the procedure and guarantees targeted radiation exposure to the tumor area.
It is important to remember: the success of radiation therapy for cancer largely depends not only on the accuracy of the equipment and the work of specialists but also on the patient themselves. During the preparation period, it is necessary to strictly observe the rules of personal hygiene, maintain a full sleep and rest regimen, and adhere to the recommended diet.
What are the possible side effects after radiation therapy?
The severity and clinical manifestation of side effects after radiotherapy depend on the location of the irradiation, the total dose, and the individual characteristics of the patient's body. The most common ones include:
- Skin reactions - redness, dryness, itching, peeling of the skin in the irradiation area; sometimes burns of varying degrees are possible;
- Fatigue - a feeling of weakness that may persist for several weeks after completing the course;
- Alopecia - hair loss in the irradiation area; in some cases, partial or late restoration of hair growth is possible;
- Nausea and vomiting - more common when irradiating organs of the abdominal cavity or pelvis;
- Appetite problems - decreased or loss of appetite, changes in taste sensations;
- Impaired function of internal organs - depending on the location of the irradiation, temporary or persistent changes in organ function are possible (e.g., lungs, digestive tract, genitourinary system);
- Problems with the hematopoietic system - a decrease in the level of white and red blood cells when irradiating the bone marrow;
- Edema and inflammatory reactions - may occur in tissues that have been irradiated;
- Long-term effects - tissue scarring and fibrosis, changes in skin pigmentation, and rare cases of secondary neoplasms years after treatment.
It is important to remember that side effects are individual: some patients experience them more strongly, while others hardly show any. The doctor always assesses the risks and selects a therapy regimen to minimize negative consequences for the body while effectively fighting the tumor.
Recommendations for patients undergoing radiation therapy
Each person's body reacts to the course of therapy differently. Treatment always puts a serious strain on the patient, so during the course, a feeling of increased fatigue is possible. In such cases, it is important to rest more and listen to your feelings - go to bed if you feel the need.
As a rule, the feeling of fatigue gradually disappears within 4–6 weeks after completing the course. However, physical activity should not be completely excluded: moderate exercise helps strengthen the body's defenses and increase its resistance to stressful influences. Specific recommendations on the type and intensity of physical exercises are best discussed with the attending physician and a physical therapy specialist.
During treatment, it is recommended to follow these rules:
Proper Nutrition
Maintain a balanced diet with an optimal ratio of proteins, fats, and carbohydrates (approximately 1:1:4). Drink sufficient fluids. This includes mineral water, juices, or tea.
Avoiding Harmful Habits
It is recommended to refrain from smoking and consuming alcohol during the course of therapy.
Clothing
Prefer loose-fitting clothing, especially on the irradiated areas of the skin. Do not wear wool or synthetic items. The ideal option is loose cotton clothing. Try to keep the irradiated areas of the body exposed.
Skin Care
After therapy, the skin sometimes becomes darker or looks slightly tanned. Sometimes by the end of treatment, these areas can become very moist, especially in skin folds, which is an individual reaction of the body. Inform your doctor about all detected changes—they will advise you on how to care for it safely.
Fresh Air
Try to go for walks more often.
Sun Protection
When going outside, protect irradiated areas from direct UV rays with clothing or hats.
Skincare Products
Do not use soap, creams, deodorants, cosmetics, or other skincare products on the irradiated areas without first consulting your doctor.
Mechanical Impact
Try not to rub or scratch the skin on the irradiated areas; do not apply heat or cold to them—no heating pads or ice.
Rehabilitation
The next stage after completing radiation therapy is the body's recovery. All actions are aimed at minimizing the consequences of therapy and supporting the patient's general condition. Properly organized rehabilitation promotes the gradual restoration of bodily functions and reduces the risk of complications.
The process is supervised by specialists who select individual rehabilitation programs, taking into account the specifics of the oncological process, the irradiation area, and the patient's individual characteristics. The timeframe for full recovery varies depending on these factors and averages from several weeks to several months.
Advantages of Radiation Therapy at Our Center in Minsk
In addition to treatment on a modern, high-precision radiotherapy system, our institution offers patients:
Assistance from a team of experienced radiation oncologists and radiologists, medical physicists, engineers, nurses, and technicians with extensive experience and professional expertise
Comprehensive support at all stages of treatment
Minimization of side effects thanks to modern methods of radiation planning and control
The possibility of outpatient radiation therapy.
Comfortable single rooms equipped with everything necessary for the convenience and peaceful stay of patients during treatment and subsequent rehabilitation.


You can schedule a primary consultation for multiple myeloma treatment by phone or by filling out the form on the website.




